
WASHINGTON, DC - JULY 25: U.S. President Joe Biden delivers remarks on expanding access to mental health care in the East Room at the White House on July 25, 2023 in Washington, DC. Biden outlined plans to expand access to mental health care by requiring health plans to make to easier to get in-network care. (Photo by Win McNamee/Getty Images)
President Joe Biden this week announced new steps to improve mental health care in America, proposing a new rule that would require private health insurance companies to offer the same level of mental health benefits that they offer for physical health benefits.
The proposed rule would strengthen enforcement of a 2008 law, the Mental Health Parity and Addiction Equity Act (MHPAEA), which sought to increase parity between physical and mental healthcare, requiring insurers to cover mental health care and substance abuse treatment the same way they cover other illnesses.
But the law has rarely been enforced, allowing insurance companies to skirt its requirements by offering few options for in-network care and providing lower rates of reimbursement to mental healthcare providers.
As a result, many providers refuse to accept insurance, making in-network mental healthcare exceedingly difficult to find and forcing many Americans to shell out hundreds of dollars per month to get out-of-network treatment—or to go without care altogether.
“As a result, folks with depression, anxiety, post-traumatic stress, bipolar disorders, eating disorders, addiction, and other illnesses often go without care,” Biden said at an event at the White House on Tuesday. “Just like when you break a bone or have a heart attack, when you’re having a mental health crisis, you should be able to get help — medical help, professional help.”
“But, right now, for millions of Americans, mental health care and treatment for substance abuse is out of reach,” he added, citing statistics showing that in 2020, fewer than half of all adults with mental illness diagnoses received care.
The rule would call on insurance companies to evaluate coverage based on a number of benchmarks, in order to “make sure people have equivalent access between their mental health and medical benefits,” according to the fact sheet. These benchmarks include the plan’s provider network, how much plans pay for out-of-network coverage and how often prior authorization is required and approved under existing plans, according to the White House.
According to the rule, these evaluations must then be followed up by action from insurance companies to improve access to care in order to comply with the law. Such action could include adding more providers to their networks or making it easier to get care by cutting red tape, according to the White House.
“Mental health care is healthcare,” Biden said Tuesday. “It’s essential to people’s wellbeing and their ability to lead a full and productive life, to find joy, to find purpose, to take care of themselves and their loved ones. It’s about dignity.”
The proposal would also make clear that health plans cannot use restrictive prior authorization requirements or erect other barriers to care that make it harder for people to use their mental health benefits than their medical benefits.
Under the proposed rule, health plans must also use similar factors to set out-of-network payment rates for mental health and substance use disorder providers as they do for medical providers.
The departments of Labor, Treasury and Health and Human Services will be tasked with enforcing the rule. Once the rule is published in the Federal Register, which the White House expects to occur next week, it will go through a 60-day public comment period before being finalized and taking effect.
The proposal is just the latest effort from the White House to address the growing mental health crisis in America. In 2022, Biden signed the Bipartisan Safer Communities Act into law, allocating roughly $10 billion in funding for mental healthcare, the largest-ever investment in America’s mental healthcare system.
Most of that funding is going towards expanding certified community behavioral health clinics (CCBHC) in every state. These clinics are required to treat patients for mental health and/or substance use issues, regardless of their insurance coverage. CCBHCs also provide 24/7 crisis response, medication-assisted treatment, and have shown promise in treating patients.
The law also included $1 billion to increase the number of mental health counselors in schools, provided additional funding for pediatric mental health care, mental and behavioral health organizations and community groups, and for the new 988 National Suicide Prevention Lifeline.
That legislation has been followed up by other steps, including a proposed rule to expand access to mental healthcare services for Medicare patients, adding Spanish text and chat services to the 988 system, and a rule that would make it easier for schools to bill Medicaid for mental health services.
“We have a moral obligation, in my view, to be there for each other, to reach out, reach to our neighbors with grief and stress and trauma and despair, reach out to them to offer help, or just a listening ear, to have the courage to ask for help when we need it, and it’s hard, because we know that even when it feels as dark as you can get, we aren’t alone. It’s important for people to realize they’re not alone,” Biden said on Tuesday. “That’s what I want, I want everyone in America not to feel isolated or alone, to know their country has their back, to know their president has their back.”
by Keya Vakil
07/28/23

Iowa Republicans make outlawing gay marriage key 2024 campaign priority
Iowa Republicans have made outlawing gay marriage a key goal in their 2024 party platform. During the Iowa GOP’s 2024 state convention on Saturday,...

Department of Justice says Iowa immigration law violates US Constitution
If Iowa doesn’t suspend the enforcement of its new immigration law by May 7, the state could face a federal lawsuit, according to the Des Moines...

Rushing: Iowa State president said the quiet part out loud
I want to thank Iowa State University President Wendy Wintersteen for doing us all a favor by finally saying the quiet part out loud: all the...

Iowa sets aside almost $180 million for year two of voucher program
Iowa has committed nearly $180 million in taxpayer funds to support private school tuition in the 2024-25 school year, which is almost $50 million...

Kalbach: Immediate action needed on corporate ag pollution
Iowa agriculture has undergone substantial changes over the past 40 years. We see it all around us. Rather than crops and livestock being raised on...
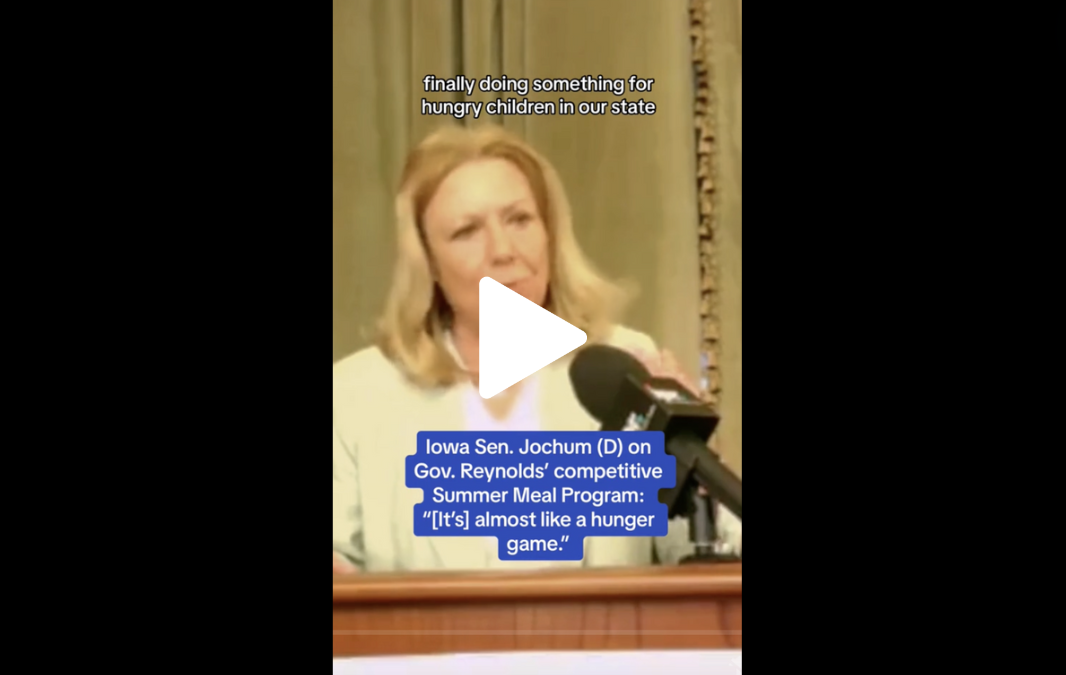
VIDEO: Jochum calls Gov. Reynolds’ summer meal program a ‘hunger game’
Iowa Gov. Reynolds announced a competitive $900,000 grant program to feed Iowa children over the summer, months after she declined $29 million in...





